DIABETIC RETINOPATHY:
WHAT IS DIABETIC RETINOPATHY?
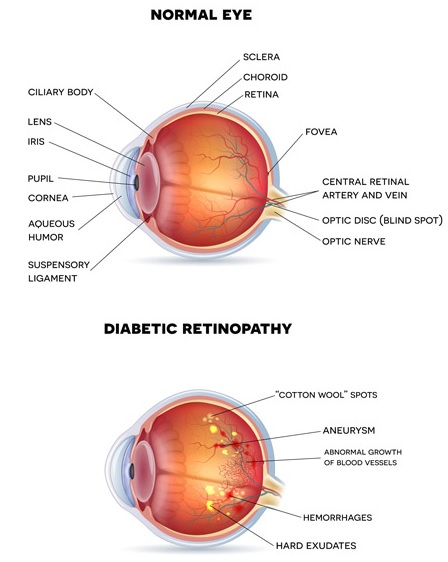
Diabetic retinopathy is one of the leading causes of severe and permanent blindness in people with diabetes which rises as a complication of diabetes. As Diabetic retinopathy is asymptomatic in the early stages, you may not notice any changes to your vision at first.
During these stages, small blood spots appear in the retina which will be able to spotd by doctor on dilated eye examination. As DR worsens over time, fragile abnormal blood vessels develop in the retina at the back of the eye and can leak blood into the central vitreous gel of the eye, obscuring vision. These blood vessels can also leak fluid into the macula, resulting in macular swelling, which causes blurring in the central part of your vision. If left untreated, secondary glaucoma, retinal detachment and irreversible blindness can result.
CAUSES, TYPES AND RISK FACTORS
People with both type 1 and type 2 diabetes are at risk of diabetic retinopathy. About 60% of patients with diabetes for 15 years of more will have DR. During pregnancy, DR may worsen in women with diabetes.
Therefore, all diabetic patients should have a comprehensive dilated eye examination on diagnosis of diabetes, followed by a repeat eye examination or a photograph of the retina at least once a year thereafter.
In the earlier stages of non-proliferative DR, blood spots and fatty deposits may be seen in the retina. These are asymptomatic and usually, do not affect vision. If left untreated, abnormal leaky blood vessels grow in proliferative DR, which leak blood and fluid to cause severe vision loss.
Secondary glaucoma and retinal detachment can occur and may result in permanent blindness.
TREATMENT
Good control of blood sugar, blood pressure and blood cholesterol levels is vital in all diabetics to reduce the risk of diabetic retinopathy. Yearly eye screening in those with good control of their diabetes is essential. Screening may need to be performed more often in newly diagnosed diabetics as well as in those whose blood sugar level control is not optimal or in women with diabetes.
Proliferative DR is treated with laser surgery to help shrink abnormal blood vessels. Often, 2 or more laser sessions are required. If severe, vitrectomy surgery may be required.
Macular swelling may also be treated with laser surgery. Treatment with Lucentis or Eylea has also been found to be beneficial.